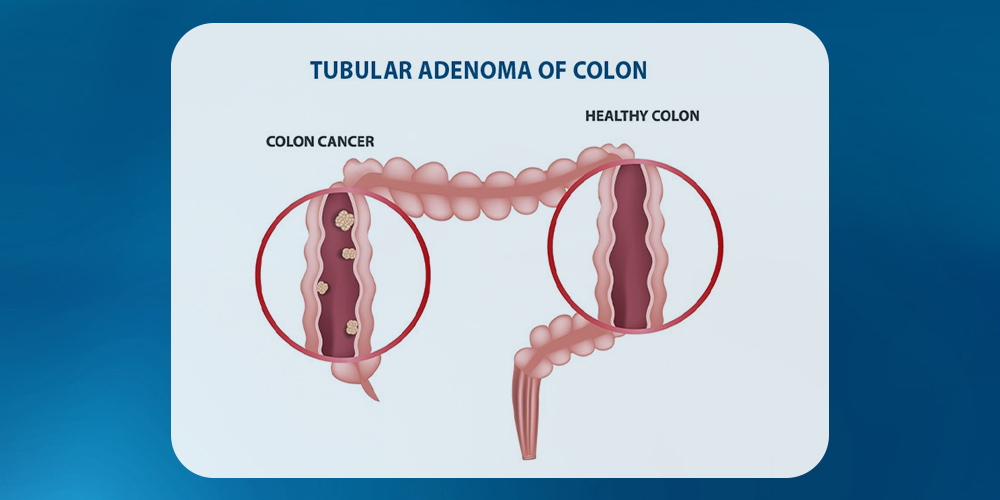
Have you ever had a colonoscopy? If so, you might have heard your doctor mention polyps, those little clumps of cells in your colon. Most of the time, they aren’t a big deal. But sometimes, they can become a problem if they turn into something more serious, like colon cancer. One of the most common types of polyps is called a tubular adenoma. These polyps are called “tubular” because of their tube-like appearance under a microscope. While most adenomas aren’t dangerous, it’s essential to monitor them, as they have the potential to turn into a severe condition.
What is Tubular Adenoma?
Tubular adenomas are often called “precancerous polyps” because they can be an early sign of colorectal cancer. Around 50% of people develop adenomas at some point in their life. Moreover, doctors commonly detect these during routine colonoscopies. Fortunately, fewer than 10% of tubular adenomas become cancerous. However, early detection of these polyps enables prompt removal solutions, significantly lowering the risk of progression to colorectal cancer.
There are some commonly referred stages of tubular adenoma of colon which can progress in distinct ways such as:
Initial Stage:
In the early tubular adenoma stage, the adenoma appears as a small, benign polyp having lower risk of malignancy.
Intermediate Stage:
Once the stage passes the polyp grows and the cellular change can increase the precancerous potential.
Advanced Stage:
Over time these can transform into colorectal cancer, this happens when the polyps grow larger (bigger than 1 cm) and have cells that look abnormal or start to act in unhealthy ways.
However, identifying and removing tubular adenomas at its earliest through regular screenings is crucial in reducing the risk of progressive cancerous condition.
Understanding the Formation of Tubular Adenoma Polyps
TA polyps occur when certain cells in the colon grow uncontrollably. This overgrowth, which is also called mutation, can lead to polyps or other types of tumors in the colon. Similarly, Phyllodes Tumors— though commonly found in the colon, can also form in other parts of the body such as the breast. This shows how changes in cells can lead to benign (non-cancerous) or precancerous growths in different tissues.
While the exact cause of these cell mutations remains unknown, experts believe this involves both genetic factors and environmental influences. In some cases, polyps develop after long-term inflammation in the colon, like in conditions such as ulcerative colitis or Crohn’s disease. These conditions can raise the risk of not only colon cancer but also other types of cancers. This inflammation doesn’t directly turn polyps into cancer, but it is prone to damage the colon lining.
As the body tries to repair this damage, it causes more cell activity, which increases the chance of developing polyps, like tubular adenomas (TA).
Recognizing Tubular Adenoma Symptoms
TAs typically don’t show noticeable symptoms, which is why they’re hard to detect without a colonoscopy. However, some people may experience symptoms like painless bleeding, where either bright or dark red blood appears after using the toilet. This can be a sign of a polyp or other colon issues that require attention.
However, some additional symptoms include:
- Frequent constipation or diarrhea
- Unexplained weight loss
- Mucus in the stool
- Signs of anemia, due to blood loss in the stool
- Reduced appetite
- Abdominal discomfort or cramps
If you experience any of these symptoms, it’s important to consult your doctor. As early detection is essential, it further helps in treatment of tubular adenoma of colon which is the key to reducing the risk of colorectal adenoma.
Causes and Risk Factors for Tubular Adenomas
Anyone can develop tubular adenomas, but there are certain factors that increase the potential risk. While the exact cause of this disease remains unclear, some specific lifestyle changes and genetic factors make them more likely to form.
These key risk factors include:
- Age: Individuals over 50 are more likely to develop tubular benign.
- Smoking and Tobacco Use: People who regularly use tobacco are more prone to develop them.
- Obesity and High BMI: With excess body weight there is a likelihood of developing colon polyps.
- Gender: Generally, men are at a greater risk than women.
- Family History: A family history of colorectal cancer or polyps doubles your risk of developing colorectal adenomas.
- Medical History: Having previous cases of colorectal cancer and conditions like inflammatory bowel disease increases the risk of developing this certain condition.
- Genetic Conditions: Certain inherited gene mutations can increase the risk of developing rare forms of colorectal cancer, such as familial adenomatous polyposis (FAP) or MUTYH-associated polyposis (MAP).
Moreover, some other factors include heavy usage of alcohol and lack of physical activity. Managing and identifying these risks are a crucial step to take in order to prevent the development of tubular benign and lower the potential for colorectal cancer.
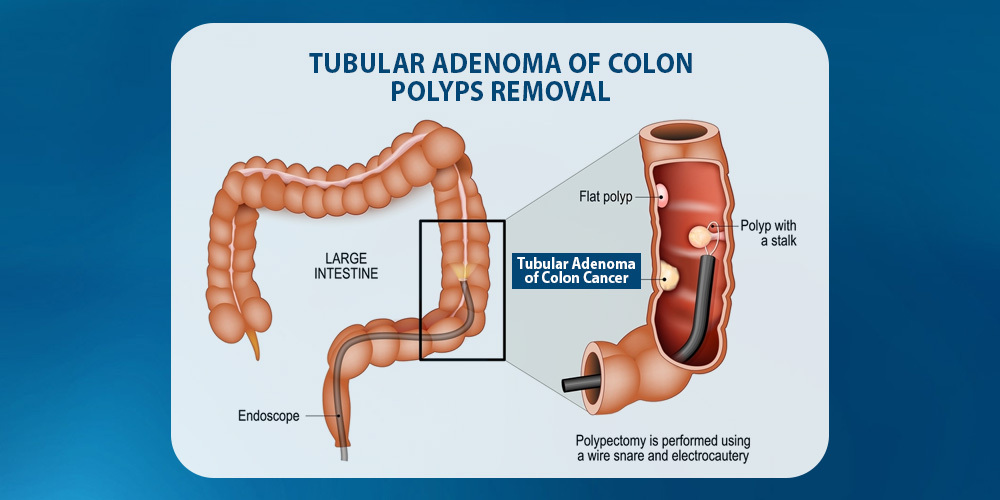
Tubular Adenomas Treatment and Management
When tubular adenomas are found, they are usually removed right away. It’s impossible to tell if a polyp is harmless or precancerous just by looking at it, which is why doctors act quickly. It is one of the most prevalent colon polyps treated by most healthcare specialists. These polyps become cancerous when they become bigger leading towards complex conditions. Moreover, some TAS are non-cancerous but can become cancerous if left untreated. Thus, it is essential to treat and remove these polyps before they can develop into cancer.
Since it’s impossible to tell if a polyp is harmless or precancerous without examining it under a microscope. So, when polyps are found during a colonoscopy and there are signs of cancer, doctors usually remove them right away. If the cancer has spread to nearby lymph nodes, a total colectomy might be necessary to improve the patient’s condition.
In cases where there’s a genetic condition, like familial adenomatous polyposis (FAP) or familial juvenile polyposis, surgery is often the best option. The exact type of surgery depends on how many polyps are present and how far they’ve spread in the colon and rectum.
- If the rectum has fewer polyps, a total colectomy (removal of the colon) with ileorectal anastomosis may be performed. This procedure connects the small intestine to the rectum, allowing for closer monitoring of the rectum.
- If the rectum is filled with polyps, complete removal of both the colon and rectum (total proctocolectomy) is often required.
For those with FAP, there are three main surgical approaches to remove the colon and/or rectum:
- Total colectomy with ileorectal anastomosis – removes the colon but keeps the rectum.
- Total proctocolectomy with ileostomy – removes both the colon and rectum and requires an external pouch.
- Restorative proctocolectomy with an internal pouch – removes the colon and rectum and creates an internal pouch for bowel movements, avoiding a permanent external bag.
These treatments aim to reduce the risk of colon cancer while allowing patients to maintain quality of life.
Is a Tubular Adenoma Cancer?
Is a Tubular Adenoma Cancer? Many people wonder if tubular adenomas, which are a type of colon polyp, are cancerous. Generally, tubular adenomas are benign growths, meaning they are not cancer, but they have the potential to develop into colorectal cancer over time if left untreated. Regular screening and removal of these polyps significantly reduce the risk of progression.
Understanding whether a tubular adenoma is cancer helps in early detection and maintaining colon health.
How Serious is a Tubular Adenoma?
A tubular adenoma is not cancer, but it is considered precancerous. You might wonder how serious is a tubular adenoma. The answer depends on several factors. While the overall risk of it turning into colorectal cancer is relatively low, that risk increases with larger size, abnormal cellular changes (dysplasia), or the presence of multiple polyps. This makes early detection and regular screenings essential for prevention.
Dysplasia in Tubular Adenomas
Dysplasia refers to abnormal changes in the cells of a tissue. When found in polyps such as tubular adenomas, it means the cells no longer look completely normal under a microscope, but they haven’t become cancerous yet.
There are two main types of dysplasia:
Low-Grade Dysplasia
Low-Grade Dysplasia refers to early, mild cell changes that are usually not cancerous but may require monitoring.
High-Grade Dysplasia
High-Grade Dysplasia reflects more advanced abnormalities that may be closer to developing into cancer.
Can Tubular Adenomas Come Back?
Once a TA is fully removed, it’s rare for it to grow back. However, about 30% of people who have had polyps removed will eventually develop new ones. That’s why it’s so important to follow through with regular colonoscopies as recommended by your doctor.
There are certain factors that can increase the chances of new polyps forming, especially if you:
- Are male
- Are over 60 years old
- Have a family history of colon polyps or colon cancer
- Have obesity or a high BMI
- Smoke or drink heavily
These factors not only increase your initial risk of developing this disease but also make it more likely to recur. However, this highlights the importance of regular screening and healthy lifestyle choices one should make.
The Significance of Oncology Clinical Trials
Oncology clinical trials are essential for improving cancer treatments by testing new therapies and approaches. These clinical trials help researchers understand the effectiveness and safety of potential treatments. For instance, solid tumor clinical trials are exploring treatments specifically for solid tumors. They help determine the effectiveness and safety of potential treatments, such as those targeting solid tumors, aiming to improve survival rates and quality of life for patients.
Conclusion:
Detecting and managing tubular adenomas is essential when it comes to preventing colorectal cancer, especially since they can become cancerous if not treated. For people with a higher genetic risk, certain medical histories, or specific lifestyle factor, taking proactive steps is even more crucial. For those with higher genetic risk, medical history, or lifestyle factors, proactive management is especially crucial. Furthermore, NHO Revive continues to expand the knowledge and treatment options of various cancers. They also provide essential support for patients dealing with various types of cancer.