Chronic Myeloproliferative Disease (CMPD) is an umbrella term for multiple disorders of the blood and bone marrow. They are categorized according to the type of blood cells affected or overproduced. Statistically, it has an incidence rate of 2.1% per year and affects people of all backgrounds. In this blog, we’re going to dive into the different kinds of chronic myeloproliferative disorders, the signs to look out for, and the treatment options available out there.
What Is Chronic Myeloproliferative Disease?
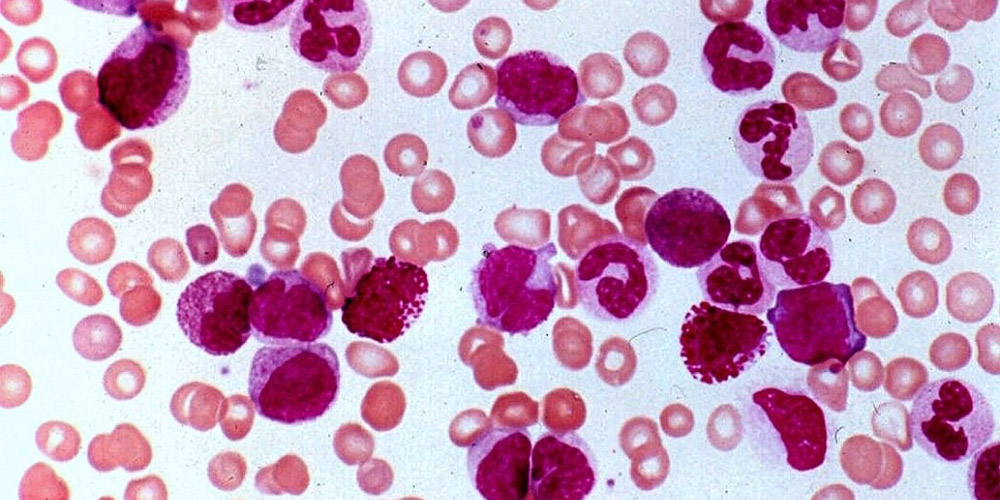
Usually, bone marrow produces just the right amount of blood cells. Over time, the immature cells grow into mature red blood cells, white blood cells, and platelets. However, during myeloproliferative neoplasms, there is excessive production of these cells, some of which are even defective or immature. This overproduction can lead to complications such as blood clots, anemia, and an enlarged spleen. Moreover, the condition also disrupts the role of the blood cell type that it attacks.
Each type of blood cell serves a unique purpose:
- Red blood cells are responsible for supplying oxygen to the body’s tissues and organs.
- White blood cells protect the body from foreign bodies such as pathogens, germs, and infections.
- Platelets are supposed to aid the formation of clots and control extra bleeding.
During myeloproliferative disease, the cells are unable to execute their function properly, resulting in some complex symptoms.
Types of Chronic Myeloproliferative Disease
MPD comes in six distinct forms. The type of blood cells your body produces in excess determines which kind you have. The common categories are:
Polycythemia Vera
In this type, there is an uncurbed production of red blood cells. Sometimes, it can also be coupled with a higher number of white blood cells and platelets.
Chronic Myelogenous Leukemia (CML)
This is the result of your bone marrow producing an excessive number of immature white blood cells.
Chronic Idiopathic Myelofibrosis
People with this condition have an accumulation of immature red and white blood cells. Consequently, the fiber web inside the bone marrow becomes inflamed and thick, resembling scar tissue. This decreases the production of red blood cells, causing anemia.
Chronic Neutrophilic Leukemia
This type results in an overabundance of neutrophils, a particular kind of white blood cell, in the patient’s blood.
Essential Thrombocythemia
During this condition, the platelets are overproduced. Hence, this causes issues with blood clotting.
Chronic Eosinophilia Leukemia
Eosinophils are an additional subset of white blood cells. These are created when the body is exposed to an allergy or parasite. These cells are abundant in the blood of those who suffer from this kind of MPD.
Also Read: Difference Between Leukemia and Lymphoma
What Causes of Chronic Myeloproliferative Disease?
Grasping the reasons behind chronic myeloproliferative disease can help clarify these complicated conditions. Mostly, genetic mutations, especially in the JAK2 gene, are involved in triggering the disease. Often, these mutations just happen on their own without any clear external cause. The Philadelphia Chromosome is especially important in chronic myelogenous leukemia, as it points to a specific genetic alteration that can affect treatment choices.
Even though genetics are a big factor, things like lifestyle and the environment can also play a part in how the disease develops. Importantly, research indicates that individuals who have been exposed to high radiation levels or certain harmful substances, such as benzene, may have a higher chance of developing conditions like polycythemia vera, primary myelofibrosis, and chronic myelogenous leukemia. Still, clinical trials for cancer are working to figure out how all these factors interact with each other.
Chronic Myeloproliferative Disease Symptoms
Although symptoms greatly depend on the type of myeloproliferative neoplasm, some common indicators are:
- Firstly, constant fatigue is a hallmark symptom.
- Secondly, there is prominent weight loss, often accompanied by loss of appetite.
- Thirdly, severs and chills are witnessed in some patients, mostly in leukemias.
- Often, patients with this syndrome bruise easily.
- Moreover, an enlarged spleen can lead to discomfort or fullness in the abdomen.
- Also, increased blood viscosity can cause headaches and feelings of lightheadedness.
- Additionally, most people with myelogenous leukemia sweat more during the nights.
- In primary myelofibrosis, there are frequent complaints of joint pain.
- Generally, patients of essential thrombocythemia report unexplained bleeding in the gums, nose, and urine.
Diagnosis of Chronic Myeloproliferative Disease
Figuring out if someone has chronic myeloproliferative disease (CMPD) takes a thorough approach. Doctors usually run blood tests, do bone marrow biopsies, and conduct genetic tests to spot specific mutations. These tests are key in distinguishing the various types of CMPD and help in deciding on the best treatment options.
For example, if a patient is diagnosed with chronic myeloid leukemia (CML), they often get tested for the Philadelphia chromosome, and this provides a route for their treatment. Getting the diagnosis right is super important since treatment methods can differ a lot among the different types of CMPD. If you want to dive deeper into the diagnosis process, you can benefit from clinical trials.
Treatment Choices for Chronic Myeloproliferative Disease
When it comes to managing chronic myeloproliferative disease, the treatment options vary based on the specific type and the unique needs of each patient. Here are some common approaches:
Medications
Hydroxyurea: This drug is used to lower the production of blood cells in conditions like polycythemia vera (PV) and essential thrombocythemia (ET).
Interferon Alpha: This type of immunotherapy can be beneficial for treating chronic myeloid leukemia (CML) and other forms of CMPD.
Tyrosine Kinase Inhibitors: For those with CML, medications like imatinib target the genetic mutations linked to the disease, especially in patients with the Philadelphia chromosome.
Blood Treatments
Some patients might need therapeutic phlebotomy to control high red blood cell counts in PV or plateletpheresis to address high platelet levels in ET. So, these procedures help lower blood cell counts and reduce the risk of complications.
Clinical Trials
Joining clinical trials for cancer can also open doors to new treatment options. These trials often investigate new drugs, therapy combinations, and other methods that might not be available yet. For individuals with chronic myelogenous leukemia, participating in Chronic Myelogenous Leukemia Clinical Trials could provide exciting alternatives to standard treatments.
Read More: How Is Leukemia Diagnosed?
Conclusion: Living with Myeloproliferative Disorder
To conclude, dealing with chronic myeloproliferative disease means you need to stay on top of your health. Regular doctor visits and blood tests are super important to keep track of how things are going and to tweak your treatment when needed. Plus, living a healthy lifestyle can boost your overall health. Therefore, surround your life with balanced meals, exercise, and ways to manage stress. Joining support groups or clinical trials can also help a lot. They offer emotional backing and practical therapies for people going through this long-term condition.