Lung cancer is one of the most common cancers worldwide, affecting millions of individuals each year. However, a question frequently asked is, “Is lung cancer hereditary?” People often worry whether their family history could increase their risk of developing the disease. While genetics can play a role, environmental factors and lifestyle choices are significant contributors to lung cancer. Therefore, this blog aims to explore the hereditary aspects of lung cancer, its causes, and the available resources, including Non-Small Cell Lung Cancer Clinical Trials, for patients and their families.
What Does It Mean for Lung Cancer to Be Hereditary?
Hereditary lung cancer means that genetic mutations passed down through family lines may increase the likelihood of developing the disease. While lung cancer is most commonly caused by smoking, exposure to environmental toxins, and other lifestyle factors, genetic predisposition can also contribute.
Research suggests that certain inherited mutations in genes like EGFR, TP53, and ALK can make some individuals more susceptible to lung cancer. However, it is essential to note that hereditary factors alone rarely cause the disease. Instead, they may increase vulnerability when combined with external factors like smoking or exposure to radon.
Types of Lung Cancer and Their Relation to Genetics
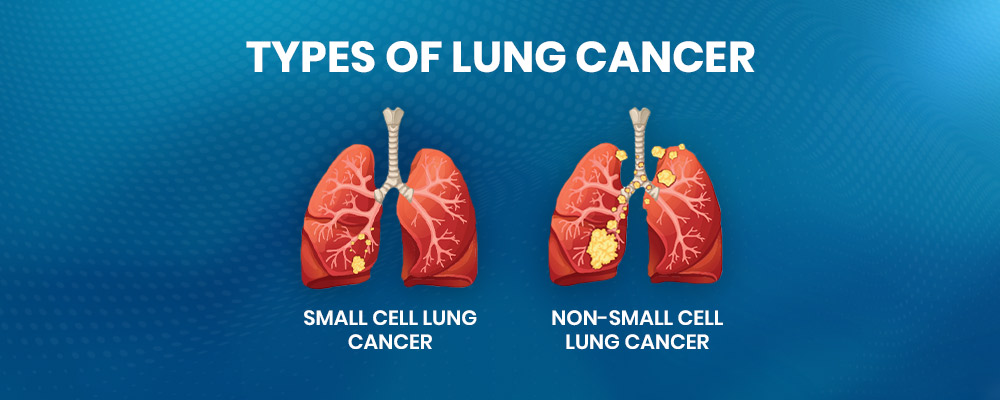
To better understand the question “Is lung cancer hereditary?”, it’s essential to look at the two primary types of lung cancer:
Non-Small Cell Lung Cancer (NSCLC):
This type accounts for about 85% of lung cancer cases. Subtypes of NSCLC include Large Cell Lung Carcinoma, adenocarcinoma, and squamous cell carcinoma. Moreover, certain genetic mutations, such as those in the EGFR and ALK genes, are more commonly seen in NSCLC patients.
Small Cell Lung Cancer (SCLC):
This more aggressive type of lung cancer spreads quickly. While genetic links exist, environmental and lifestyle factors are the primary causes.
Another unique form of lung cancer to consider is the Pancoast Tumor, which grows at the top of the lung. However, genetic predisposition to lung cancer could potentially play a role in its development, especially when combined with lifestyle risk factors.
Genetic Mutations Associated with Lung Cancer
Several inherited genetic mutations may increase the risk of lung cancer. While not all are directly hereditary, they are often passed down in families. Some of the most notable mutations include:
- EGFR Mutations: Found in a subset of lung cancer patients, particularly non-smokers with adenocarcinoma.
- TP53 Mutations: Common in various cancers, including lung cancer, and often linked to hereditary cancer syndromes.
- ALK Gene Rearrangements: Frequently seen in NSCLC, particularly in younger patients and non-smokers.
These mutations are not guarantees of developing lung cancer but increase susceptibility, especially when combined with environmental triggers.
How to Determine If You Are at Risk?
For individuals with a family history of lung cancer, understanding personal risk is crucial. While the question “Is lung cancer hereditary?” cannot always be answered definitively, the following steps can help determine risk:
- Genetic Testing: Testing for inherited mutations like EGFR, TP53, and ALK can provide insight into susceptibility.
- Family Medical History: Documenting cancers in close relatives can help identify patterns.
- Lifestyle Assessment: Factors like smoking, exposure to secondhand smoke, and occupational hazards also significantly impact risk.
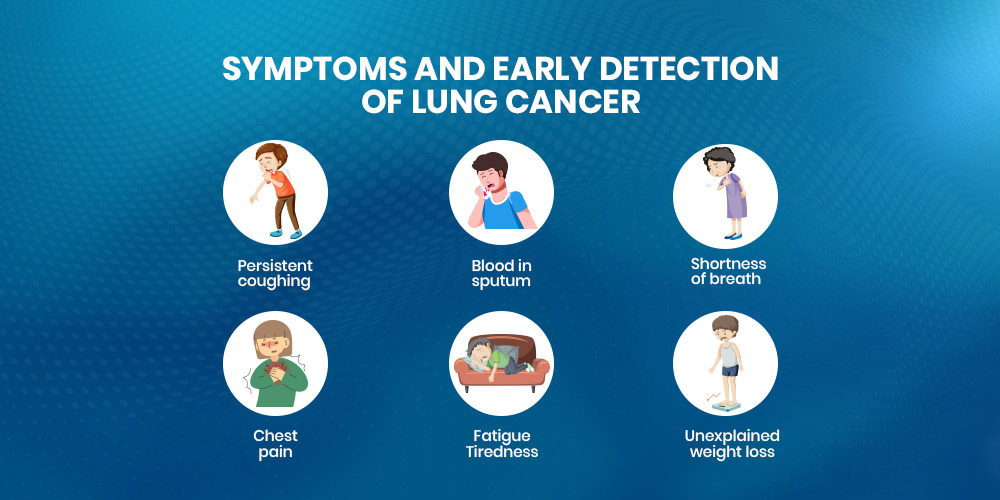
Symptoms and Early Detection of Lung Cancer
Early symptoms of lung cancer can often go unnoticed, making regular screenings essential for those at higher risk. Common symptoms include:
- Persistent coughing
- Blood in sputum
- Shortness of breath
- Chest pain
- Fatigue
- Unexplained weight loss
Moreover, screening methods such as low-dose CT scans can detect lung cancer early, especially for individuals with a genetic predisposition or a history of smoking.
Lifestyle and Environmental Factors: The Bigger Picture
While hereditary factors play a role, they account for only a small percentage of lung cancer cases. However, lifestyle choices and environmental exposures remain the primary contributors:
- Smoking: Smoking is the leading cause of lung cancer and interacts with genetic predispositions to increase risk.
- Radon Exposure: Radon gas, a natural radioactive substance, is the second leading cause of lung cancer.
- Air Pollution: Long-term exposure to polluted air can contribute to lung cancer, even in non-smokers.
Additionally, for those with a genetic predisposition, avoiding these factors is critical to reducing overall risk.
Current Research and Clinical Trials
Advances in lung cancer research are shedding light on the hereditary aspects of the disease. Nevertheless, genetic testing is becoming a standard part of diagnosis and treatment planning. However, participation in Non-Small Cell Lung Cancer Clinical Trials allows patients to access cutting-edge therapies targeting specific genetic mutations.
Additionally, ongoing research is improving our understanding of the interaction between genetics and lifestyle factors, providing more personalized prevention strategies.
Treatment Options for Lung Cancer
Treatment for lung cancer depends on the stage, type, and genetic profile of the tumor. However, the most common options include:
- Targeted Therapy: Drugs designed to attack specific genetic mutations, such as EGFR inhibitors, are effective for patients with hereditary mutations.
- Immunotherapy: Treatments that boost the body’s immune response against cancer cells are showing promise in clinical trials.
- Surgery and Radiation: These are often used in combination for localized tumors, such as those seen in the Pancoast Tumor.
Moreover, participation in research studies can provide patients with access to innovative treatment options while contributing to scientific advancement.
The Role of Family History in Prevention
Family history is a significant factor in understanding “Is lung cancer hereditary?” While you cannot change your genetics, knowing your risk can help take proactive measures. Steps to reduce risk include:
- Avoiding smoking and exposure to secondhand smoke.
- Regular screenings for those with a family history of lung cancer.
- Maintaining a healthy lifestyle to improve overall immunity.
Additionally, engaging in educational initiatives and joining support groups can also provide valuable resources for families with hereditary cancer risk.
Related Cancers and Shared Risk Factors
Certain hereditary factors may increase the risk of related cancers, such as Large Cell Lung Carcinoma and other forms of lung cancer. However, understanding the shared risk factors can help in early detection and prevention efforts.
Similarly, cancers like Neuroendocrine Cancer may share some genetic links, highlighting the importance of comprehensive genetic testing and family history documentation.
Hereditary Lung Cancer: Myths and Facts
Nevertheless, there are many misconceptions surrounding hereditary lung cancer. However, here are some clarifications:
- Myth: A family history guarantees lung cancer.
- Fact: Genetics only increases risk, not certainty.
- Myth: Only smokers develop lung cancer.
- Fact: Non-smokers with genetic predispositions can also develop the disease.
- Myth: Hereditary lung cancer is untreatable.
- Fact: Advances in research and Clinical Trials for Oncology offer hope for effective treatment.
Also Read: What Type of Cancer Causes Low Hemoglobin
Conclusion
The question “Is lung cancer hereditary?” does not have a straightforward answer, as genetics play a role but are not the sole cause. Additionally, a combination of inherited mutations, lifestyle factors, and environmental exposures determines individual risk.
While hereditary factors like EGFR (kidney filtration rate) and TP53 mutations can increase susceptibility, lung cancer prevention relies heavily on avoiding smoking, reducing exposure to environmental toxins, and undergoing regular screenings. Nonetheless, advancements in clinical research, including participation in Non-Small Cell Lung Cancer Clinical Trials, offer hope for improved treatments and outcomes.
Moreover, by understanding the hereditary aspects of lung cancer and taking proactive steps, individuals and families can reduce their risk and improve overall health outcomes. Whether exploring treatment options for a Pancoast Tumor or participating in research studies, staying informed is the first step toward a healthier future.







