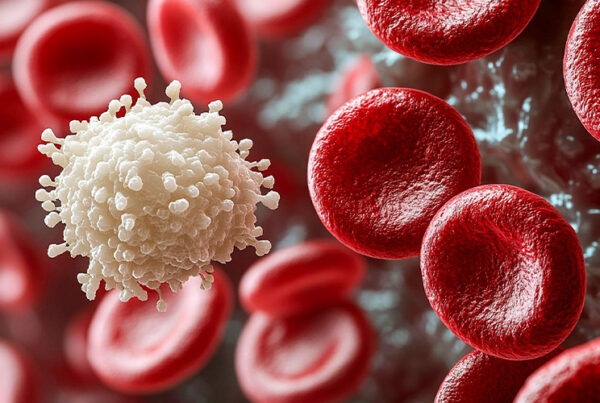
Lymphoproliferative disorders (LPDs) are a large group of conditions that impact your white cells. The lymphoproliferative disorder is the umbrella term used to define excessive production of lymphocytes. The uncontrollable growth of the white cells can lead to serious conditions like lymphoid blood cancers like lymphoma and leukemia. This disorder often arises due to immune system disorder complications, infections, or genetic factors.
Furthermore, knowing about what are Lymphoproliferative disorders is necessary as an early diagnosis and proper Lymphoproliferative disorder treatment can improve outcomes exponentially.
What are the Types of Lymphoproliferative Disorders?
There are two types of these disorders: immunological disorders and type of white blood cells. These include both B and T cell cancers.
Immunological Disorders
Immunologic disorders disrupt how your immune system responds to threats. As a result, individuals with these lymphoproliferative disorders (LPDs) face a higher risk of developing lymphoma.
- X-linked lymphoproliferative disorder (XLP): When exposed to the Epstein-Barr virus, individuals with XLP are more likely to develop lymphoma due to their immune system’s inability to control the virus effectively.
- Autoimmune lymphoproliferative syndrome (ALPS): This condition causes an excessive buildup of lymphocytes in the lymph nodes, spleen, and liver. Over time, these organs become enlarged, leading to further complications.
- Post-transplant lymphoproliferative disorders (PTLD): Though rare, PTLDs are severe complications that can arise after solid organ or allogeneic stem cell transplants. Moreover, they occur when either the recipient or the donor carries Epstein-Barr virus-infected B cells, which may trigger uncontrolled lymphocyte growth.
Additionally, by understanding these disorders and their potential risks, individuals can seek timely medical intervention and explore effective management strategies.
Lymphoid Blood Cancers
Lymphoid blood cancers occur when white blood cells undergo abnormal changes, leading to uncontrolled multiplication within the bone marrow and bloodstream. These affected cells include B-cells, T-cells, and natural killer (NK) cells. Furthermore, healthcare professionals often refer to these conditions as lymphocytic disorders. While some of these diseases are treatable, they remain serious and can be life-threatening.
B-Cell Lymphomas
Several non-Hodgkin lymphomas fall under lymphoproliferative disorders. Some of the most common types include:
- Diffuse Large B-cell lymphoma
- Follicular Lymphoma
- Mantle Cell Lymphoma
B-Cell Lymphocytic Leukemias
B-cell leukemias also fall under lymphoproliferative disorders and include the following:
Chronic Lymphocytic Leukemia (CLL):
In this condition, abnormal B-cells multiply within the bone marrow, crowding out healthy blood cells and platelets, which can weaken the immune system.
B-Cell Prolymphocytic Leukemia:
This disorder occurs when malignant B-cells form in the bone marrow, leaving little room for normal blood cells and platelets, leading to complications like anemia and infections.
Hairy Cell Leukemia:
A rare type of leukemia in which abnormal white blood cells accumulate in the bone marrow. Moreover, under a microscope, these cells appear “hairy,” giving the condition its name.
T-Cell Lymphomas
T-cell lymphocytic disorders are generally categorized into systemic and cutaneous T-cell lymphomas:
Systemic T-Cell Lymphomas:
These cancers spread throughout the lymph nodes, spleen, bone marrow, blood, and other organs, making them more aggressive and difficult to treat.
Cutaneous T-Cell Lymphomas:
Primarily affecting the skin, these lymphomas can sometimes extend to the lymph nodes, blood, bone marrow, and internal organs, requiring specialized treatment.
Additionally, understanding lymphoid blood cancers is essential for early detection and better treatment outcomes. Seeking timely medical care can make a significant difference in managing these conditions effectively.
Lymphoproliferative Disorder Symptoms
Lymphoproliferative disorder symptoms depend on the type of disorder that a person is having. However, some common ones include:
- Weakness
- Anemia
- Elevated white cell count
- Swollen lymph nodes
- Spleen or liver enlargement
- Atypical bleeding or bruising
- Weight loss
- Excessive bleeding
- Night sweats
- Bone pain
- Rashes
- Frequent infections
Additionally, organ-specific symptoms include:
- Enlarged spleen (splenomegaly) causes abdominal pain and discomfort.
- Skin rashes are common in ALPS and certain lymphomas.
- Breathing difficulties when lymph nodes press on the lungs.
- Bone pain in advanced cases affecting bone marrow.
If these lymphoproliferative disorder symptoms persist, seeking medical attention is necessary.
Diagnosis and Tests
There are multiple types of LPDs, so the diagnosis mainly revolves around identifying the true cause of the disease.
To diagnose the condition, a healthcare provider will evaluate symptoms such as swollen cervical lymph nodes and any enlargement of the liver or spleen. They will also review your medical history to identify potential risk factors.
To confirm the diagnosis, they may recommend the following tests:
- Biopsy: A bone marrow biopsy may be performed to check for signs of blood cancer, such as leukemia or lymphoma.
- Blood Tests: These may include a complete blood count (CBC), comprehensive metabolic panel (CMP), Epstein-Barr antibody test, hepatitis screening, HIV test, and lactate dehydrogenase (LDH) test.
- Imaging Tests: Diagnostic imaging, such as computed tomography (CT) scans and positron emission tomography (PET) scans, can help assess the extent of the disease.
- Laboratory Tests: A flow cytometry test may be conducted to identify specific immune system disorders and confirm the diagnosis.
By using a combination of these tests, healthcare providers can determine the best course of action for treatment and management.
When to See a Doctor?
Anyone experiencing prolonged lymphoproliferative disorder symptoms should consult a healthcare professional. Furthermore, early diagnosis often leads to better outcomes, and clinical advancements in lymphoproliferative disorder treatment continue to improve survival rates.
A physician may prescribe the following tests:
- Blood tests: To detect abnormal lymphocyte counts.
- Biopsies: To analyze affected tissues.
- Imaging scans: To identify tumor locations.
Conclusion
To conclude, Lymphoproliferative Disorder includes various conditions affecting lymphocyte growth. Understanding What are lymphoproliferative disorders helps in recognizing symptoms early and seeking appropriate lymphoproliferative disorder treatment.
Furthermore, as research continues, advancements in Clinical Trials of Mantle Cell Lymphoma, Follicular Lymphoma Clinical Trials, and other studies are offering new hope for patients.
Additionally, if you or someone you know experiences persistent lymphoproliferative disorder symptoms, consulting a medical professional is essential. Early detection and treatment can make a significant difference in managing Lymphoproliferative Disorder effectively.
Furthermore, NHO Revive, which has decades of clinical experience and innovative research, is eager for you to join its experiment. We strive for greatness by offering the best patient care possible along with a strong desire to help others. Moreover, to help us carry out innovative clinical trials, all we need is your involvement.
Frequently Asked Questions
Is lymphoproliferative disorder cancer?
Some lymphoproliferative disorders are classified as lymphoid blood cancers, while others are immune system disorders that may lead to cancer.
How long can you live with lymphoproliferative disorder?
Life expectancy varies depending on the type, severity, and treatment response, with some cases being chronic but manageable, while others may be aggressive.
How are lymphoproliferative disorders diagnosed?
Diagnosis involves a physical exam, medical history review, blood tests, imaging scans, biopsies, and specialized lab tests like flow cytometry.
Can lymphoproliferative disorders be cured?
Some types can be treated successfully with immunotherapy and chemotherapy, or stem cell transplants, while others require lifelong management.