
Introduction:
Adenoid Cystic Carcinoma, more commonly known as ACC, is a rare and insidious form of cancer that most often arises in glandular tissues — especially the salivary glands. Understanding this disease is critical, because it grows slowly, it has a high tendency to recur and spread over time.
What Is Adenoid Cystic Carcinoma?
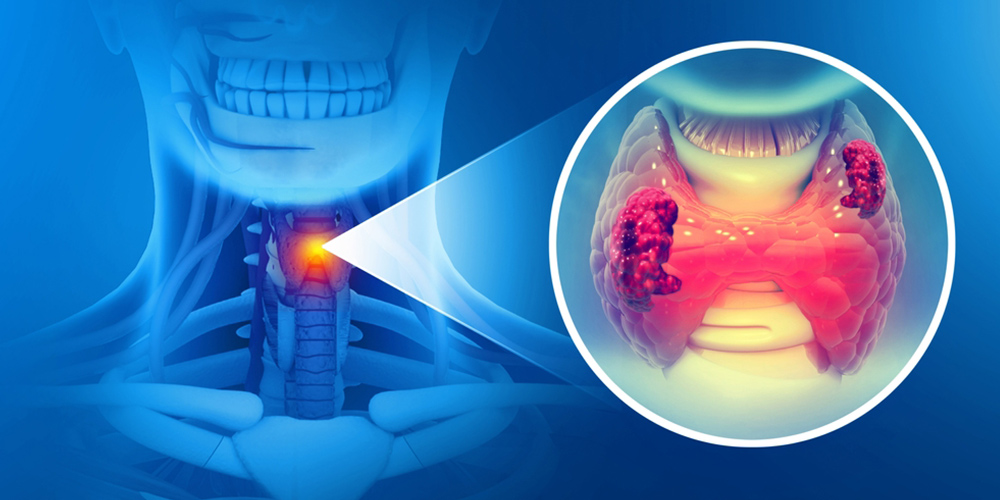
Adenoid Cystic Carcinoma (ACC) is a malignant salivary tumor that arises from glandular tissue. Though rare, it’s one of the more well-known malignant salivary tumors because of its unique behavior.
ACC most often develops in the salivary glands, but it’s not limited to those: it can originate in the parotid gland, submandibular gland, sublingual gland, as well as in other tissues like the lacrimal (tear) glands, skin, airway (trachea), or even in the breast.
Because of its slow but relentless growth, ACC is sometimes referred to as a “chronic cancer.”
Adenoid Cystic Carcinoma Symptoms
The symptoms of ACC depend heavily on where the tumor is located.
- A painless lump in the mouth, face, or neck (especially for salivary gland tumors)
- Numbness, facial weakness, or drooping due to nerve involvement (because ACC frequently invades nerves)
- Difficulty swallowing or opening the mouth
- Hoarseness, changes in speech, or throat discomfort if the tumor is in the larynx or airway
- Nasal congestion or nosebleeds if the tumor is in nasal or sinus regions
- Pain, particularly because ACC often exhibits perineural (nerve) invasion, causing nerve pain or paralysis.
- Vision changes in very late disease if in the lacrimal gland) or breathing issues if in the trachea may appear.
Because ACC is slow-growing, symptoms often develop very gradually or may not appear until the disease is advanced.
Adenoid Cystic Carcinoma Causes
The exact causes of ACC remain unclear. Medical experts believe it is linked to genetic mutations rather than inherited traits.
- A well-known feature in ACC is a fusion between two genes, often producing excess MYB protein, which seems to drive tumor growth.
- These gene changes are generally somatic, meaning they happen during a person’s lifetime (not inherited) and may be influenced by environmental factors.
- Potential contributors include exposure to carcinogens like tobacco, asbestos, or even workplace chemicals, though the evidence is not definitive.
Because there are no clearly established risk factors (like strong lifestyle links or familial inheritance), ACC remains unpredictable in many cases.
Stage 4 Adenoid Cystic Carcinoma
Staging is vital in cancer because it helps guide treatment. While specific staging systems may vary, Stage 4 ACC usually indicates advanced disease: cancer has grown beyond the original site, possibly involving:
- Nearby structures such as bone or nerves
- Distant metastasis (spread), especially to the lungs, liver, or bones
- Despite being advanced, ACC does not often spread to lymph nodes: lymph node involvement is rare (<5–10%) in many documented cases.
Because of its tendency for perineural invasion (nerve spread) and distant metastasis, Stage 4 ACC can be particularly challenging to manage.
Adenoid Cystic Carcinoma Treatment
Treatment of ACC is multifaceted and depends on the tumor site, size, stage, and whether it has metastasized. Here are the common treatment strategies:
Surgery
The first-line treatment is often surgical resection, aiming to remove the tumor with “clear margins” (no cancer cells left on the edges). And because ACC often invades nerves, surgery can be complex and may require removing part of a nerve, leading to functional or cosmetic impacts. Reconstruction may be needed, especially if vital structures are involved.
Radiation Therapy
Often used after surgery (postoperative radiotherapy, or PORT) to eliminate residual microscopic disease, especially when margins are close or positive, techniques include:
- Conventional external-beam radiation
- Intensity-modulated radiation therapy (IMRT)
- Proton beam therapy
Radiation helps improve local control, especially when complete tumor removal is not possible.
Chemotherapy / Systemic Therapy
ACC is notoriously resistant to traditional chemotherapy; it tends to respond poorly to standard cytotoxic drugs. Researchers are investigating targeted therapies (e.g., tyrosine kinase inhibitors) in clinical trials.
Solid Tumor Clinical Trials & Research
Given the limitations of standard therapy, many patients with ACC are offered participation in clinical trials — especially for solid tumor clinical trials. Clinical research studies play a vital role in advancing its treatment. Here’s why clinical trials for oncology — including for ACC — are so important:
Benefits of Clinical Research
- Patients can access new therapies that might not yet be widely available.
- Researchers can test drugs targeted to the molecular drivers of ACC (e.g., MYB fusion).
- Data from trials helps define better standards of care for rare cancers.
- Participation supports future patients, contributing to collective understanding.
Solid Tumor Clinical Trials
- Many trials categorize ACC under “solid tumor” protocols, given its origin in glandular, non-hematological tissue.
- These trials often test targeted agents, immunotherapy, or novel radiation techniques.
Clinical Research Studies in Nebraska
NHO revive research institute has a cancer clinical trials program that helps advance innovation and improve outcomes of solid tumor treatment. Participation by local patients contributes to important research and provides patients with access to novel treatments.
Living with Adenoid Cystic Carcinoma: Quality of Life and Long-Term Management:
Living with Adenoid Cystic Carcinoma (ACC) often becomes a long-term journey, as this rare cancer grows slowly but can recur or spread many years after initial treatment. For many patients, maintaining quality of life means managing chronic symptoms such as nerve pain, dry mouth, facial weakness, swallowing difficulties, or fatigue—often with the help of speech therapy, pain specialists, physical therapy, or dentist’s familiar with radiation-related side effects. Emotional well-being is equally important, since ongoing monitoring and uncertainty about recurrence can create anxiety or stress. Regular follow-up scans, lifelong surveillance, and awareness of new clinical trial options are essential parts of long-term management. Through a supportive care team, healthy lifestyle adjustments, and ongoing communication with medical providers, individuals with ACC can continue to live meaningful, fulfilling lives while navigating the challenges of chronic cancer.
Conclusion:
Adenoid Cystic Carcinoma is a complex, rare, and challenging cancer. As a solid tumor in salivary glands, it’s characterized by slow growth and a tendency to recur or spread, often via nerves or distant organs. While surgery followed by radiation therapy remains the cornerstone of treatment, long-term outcomes vary widely. Clinical trials remain a beacon of hope, offering new targeted or systemic therapies.
FAQs
1. What is the survival rate for adenoid cystic carcinoma?
- The 5-year survival rate is roughly 80%, according to clinical data.
- The 10-year survival rate drops to about 61%, and the 15-year survival may be closer to 30%, depending on studies.
- Long-term studies (20+ years) show that while local control might decline, many patients live for many years.
2. How serious is adenoid cystic carcinoma?
It’s rare, but serious: ACC is malignant, tends to invade nerves (perineural), and often recurs. And even though it grows slowly, its capacity for distant metastasis (especially lungs) makes long-term risk significant. Because of its unpredictable nature, it’s often managed like a chronic disease, with ongoing follow-up.
3. What are the symptoms of adenoid cystic cancer?
Commonly, it’s a painless lump in the face, neck, or mouth. Often people report numbness or weakness in the face due to nerve involvement. There is also difficulty swallowing, hoarseness, nasal issues, or eye symptoms, depending on tumor site. Pain may develop, especially when cancer invades nerves.
4. How fast does adenoid cystic carcinoma spread?
ACC typically grows slowly. However, despite slow growth, it often recurs many years after treatment. Spread (metastasis) tends to be via the bloodstream (especially to lungs) rather than lymph nodes, though perineural spread (along nerves) is very common.







