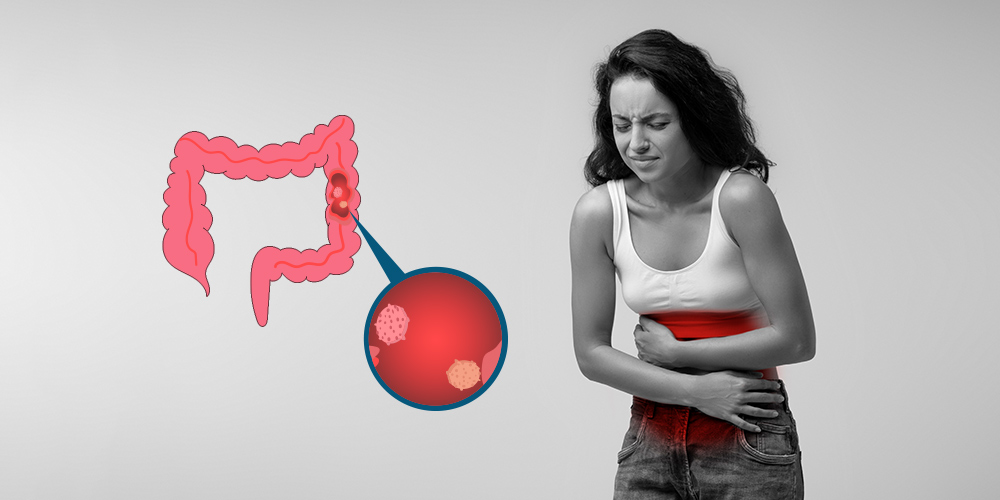
Hearing the term tubular adenoma of colon during a routine colonoscopy report can be unsettling. Many people instantly associate it with cancer, which naturally leads to anxiety and questions about what it truly means. The good news is that while this type of polyp has the potential to become cancerous, it isn’t cancer itself.
This blog aims to clarify how serious a tubular adenoma really is, what it means for your health, and the steps you can take to stay protected.
What is a Tubular Adenoma?
A tubular adenoma of colon is a type of polyp, or small growth, that forms on the inner lining of the colon or rectum. It’s considered precancerous, meaning it isn’t cancer, but it has the potential to turn into colorectal cancer over time if left untreated.
These growths are usually found during routine colonoscopies and are one of the most common types of adenomatous polyps. While they often cause no symptoms, their detection is important because of their risk of progressing into something more serious.
Tubular adenomas typically develop due to abnormal cell growth in the colon lining. Several factors can increase your risk of developing them, including:
- Age (especially over 50)
- A family history of colorectal cancer or polyps
- A diet low in fiber and high in red or processed meats
- Lack of physical activity
- Obesity and smoking
Early detection and removal of these polyps can significantly reduce the risk of colorectal cancer.
Is a Tubular Adenoma Cancer?
Is a Tubular Adenoma Cancer? To understand if a tubular adenoma could become cancerous, it helps to compare it with other types of polyps:
- Tubular adenomas mainly consist of tube-shaped glands.
- Villous Adenomas feature long, finger-like projections.
- Tubulovillous adenomas display characteristics of both tubular and villous types.
Tubular adenomas are usually small, measuring less than half an inch. In contrast, villous adenomas have a spread-out growth pattern, making them larger, faster-growing, and more likely to contain cancerous cells. Villous and tubulovillous adenomas together account for about 15% of colon polyps.
What Makes It Serious? Key Risk Factors
While a tubular adenoma is not cancer, certain features can increase its potential to become cancerous. Understanding these risk factors can help you and your doctor determine how closely the polyp needs to be monitored or whether further treatment is necessary.
1. Size of the Adenoma
One of the most important risk factors is size. The larger the polyp, the greater the risk it could turn into cancer. Polyps under 1 centimeter in diameter typically have a low risk, but once they grow beyond that, especially over 2 centimeters, the chances of cancerous changes increase significantly.
2. Number of Polyps Found
Finding more than one adenoma during a colonoscopy raises concern. Multiple polyps suggest a higher likelihood of abnormal cell growth and may point to an underlying tendency to develop them. This often results in more frequent follow-up screenings to monitor for new growths.
3. Presence of High-Grade Dysplasia
Dysplasia refers to abnormal cell development. If a tubular adenoma shows high-grade dysplasia, it means the cells already display changes that resemble early cancer. While it’s not cancer yet, this is a serious warning sign, and the polyp must be removed and closely monitored.
4. Personal and Family History of Colorectal Cancer
If you or a close relative (such as a parent or sibling) has had colorectal cancer or multiple adenomas, your risk increases. A family history may indicate a genetic predisposition, such as familial adenomatous polyposis (FAP) or Lynch syndrome, which require earlier and more frequent screenings.
How Likely Is It to Turn Into Cancer?
Understanding the likelihood of a tubular adenoma progressing to colorectal cancer—and the factors that influence this risk—is essential for effective prevention and timely treatment.
Statistics on Progression to Colorectal Cancer
Studies suggest that about 10% of tubular adenomas eventually develop into colorectal cancer if they are left untreated. This risk is relatively low compared to other adenoma types (like villous or tubulovillous), but it’s still enough to take seriously—especially because polyps often grow silently without symptoms.
Average Timeline for Potential Progression
The progression from a benign tubular adenoma to full-blown colorectal cancer typically takes 10 to 15 years. This slow growth allows a generous window for early detection and removal, which is why routine colonoscopies are so effective at preventing cancer.
Factors That Increase the Risk
- Polyp size over 1 cm
- Presence of high-grade dysplasia (abnormal cells)
- Multiple polyps found
- Family history of colorectal cancer
- Delayed or missed follow-up screenings
Factors That Reduce the Risk
- Early detection and complete removal of the polyp
- Regular surveillance colonoscopies
- Healthy lifestyle habits, including a fiber-rich diet, regular exercise, avoiding tobacco, and limiting red and processed meats
What Happens After It’s Found?
Finding a tubular adenoma during a colonoscopy can feel alarming, but it’s actually a positive step—it means the polyp has been discovered early before it has had a chance to turn into something more serious. Here’s what typically happens next:
1. Polyp Removal During Colonoscopy
In most cases, the tubular adenoma is completely removed during the same colonoscopy in which it’s discovered. This procedure is known as a polypectomy and is usually painless. Removing the polyp eliminates the immediate risk and prevents potential progression to cancer.
2. Importance of Biopsy and Pathology Report
Once the polyp is removed, it’s sent to a lab for a biopsy. A pathologist examines the tissue under a microscope to determine the type of polyp and whether any of the cells are abnormal or precancerous.
- This pathology report tells your doctor what kind of polyp you have.
- It also explains whether any of the cells look abnormal or precancerous.
- The term “dysplasia” means there are abnormal cells that could potentially turn into cancer over time.
- If the cells don’t look very abnormal, the report will say “low-grade dysplasia” — this means the risk is lower.
- If the cells look more unusual and closer to cancer, it’s called “high-grade dysplasia” — this means the risk is higher and needs closer attention.
This pathology report plays a crucial role in deciding what follow-up care is needed.
3. Recommended Follow-Up Intervals
The follow-up schedule depends on the size, number, and type of polyps found, as well as the biopsy results. Common guidelines include:
- If one or two small (<1 cm) tubular adenomas are found: A repeat colonoscopy is usually recommended in 7 to 10 years.
- If larger, multiple, or high-risk polyps are found: Follow-up may be recommended in 3 years or less.
Your doctor will tailor the follow-up plan based on your overall risk and personal health history.
Exploring Further Options and Research
Understanding the benefits of clinical research is crucial, as it paves the way for new therapies and personalized treatment options. Specifically, clinical trials for oncology bring hope by advancing cancer care and providing access to innovative treatments.
Currently, various studies are underway, including solid tumor clinical trials and Colorectal Cancer clinical trials.
If you’re interested, enrolling in clinical research studies in Nebraska offers a chance to support medical progress while receiving expert care during your participation.
Conclusion:
Tubular adenomas, although not cancerous, require careful monitoring because they can develop into colorectal cancer. Early detection, removal, and regular screenings greatly reduce this risk. Staying informed and exploring clinical trials for oncology can provide valuable treatment options and support for better health outcomes.