Blood cancer threatens the most crucial component of human existence- our blood cells. These cells give us energy, help fight infections, and prevent excessive bleeding. So naturally, when they become cancerous, the whole body suffers.
But thanks to clinical research and healthcare technology, there are many safe and effective ways to treat blood cancer today.
What is Blood Cancer?
Blood cancer hampers your body’s blood cell production and functioning.
Most blood cancers start in your bone marrow, the soft, spongy tissue inside the cavity of your bones. Your bone marrow makes stem cells that mature into white blood cells, red blood cells, and platelets.
Blood cancer happens when something disrupts how your body makes blood cells. Healthy blood cells fight infection, transport oxygen, and control bleeding. If you have blood cancer, cancerous blood cells overpower the healthy ones, resulting in a series of medical abnormalities.
Is Blood Cancer curable?
Yes, blood cancer is curable. More and more people are now able to survive and live longer with blood cancer. All thanks to the advancements in medical technology.
While blood cancer is still a very serious illness, other cancer types are more fatal. Blood cancer accounts for about 10% of all cancer diagnoses in the US, but only around 3% of cancer-related deaths.
According to the National Cancer Institute (NCI), deaths from blood cancer have been steadily declining, largely due to early diagnosis and better treatment options.
What are the Types of Blood Cancer?
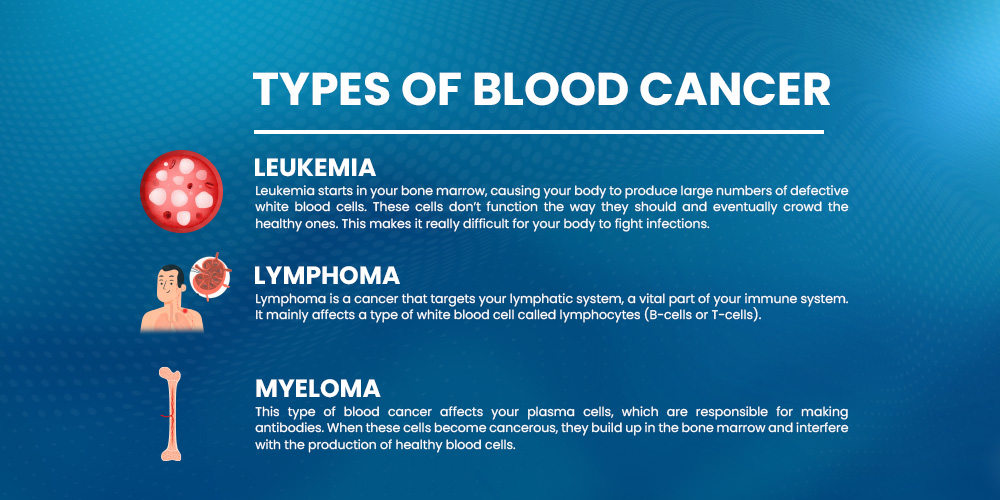
Blood cancers are categorized on the basis of the type of blood cell they affect and how they grow. There are three main types of blood cancer, further divided into types and subtypes.
Here’s a quick breakdown:
1. Leukemia
Leukemia starts in your bone marrow, causing your body to produce large numbers of defective white blood cells. These cells don’t function the way they should and eventually crowd the healthy ones. This makes it really difficult for your body to fight infections. Leukemia can be:
- Acute Leukemia (fast growing)
- Chronic Leukemia (slow growing)
- Philadelphia Chromosome Leukemia is a specific type of leukemia caused by a gene mutation, and it’s often linked to chronic myeloid leukemia (CML).
2. Lymphoma
Lymphoma is a cancer that targets your lymphatic system, a vital part of your immune system. It mainly affects a type of white blood cell called lymphocytes (B-cells or T-cells). There are two main types:
- Hodgkin Lymphoma: It usually starts in the lymph nodes around the neck, chest, or armpits and spreads in a very organized way. It is identified by a unique cell called the Reed-Sternberg cell, which doctors can see under a microscope.
- Non-Hodgkin Lymphoma: It can appear in different parts of the body, not just the lymph nodes, and may grow quickly or very slowly depending on the specific type.
Hodgkin vs Non-Hodgkin Lymphoma
The main difference between Hodgkin vs Non-Hodgkin Lymphoma lies in the specific type of cells involved. Hodgkin lymphoma has Reed-Sternberg cells, while non-Hodgkin does not.
Hodgkin lymphoma tends to spread in a more orderly fashion and often responds well to treatment. Non-Hodgkin lymphoma, on the other hand, is more unpredictable because it includes many subtypes, some of which are more challenging to treat.
Here are some common types of Non-Hodgkin lymphoma:
- Follicular Lymphoma: A slow growing type that’s often found during routine check-ups. It’s more common in older adults.
- Marginal Zone Lymphoma: Another slow-moving form that usually starts in areas like the spleen or certain lymph nodes.
- T-Cell Lymphoma: A rare and aggressive non-Hodgkin subtype that originates from T-cells, often affecting skin or other organs.
3. Myeloma
Multiple Myeloma is a type of blood cancer affects your plasma cells, which are responsible for making antibodies. When these cells become cancerous, they build up in the bone marrow and interfere with the production of healthy blood cells.
There are few forms you should know about:
- Smoldering Multiple Myeloma: This is an early, symptom free stage that still carries high a risk of progressing into active disease.
- Active Multiple Myeloma: In this stage, symptoms like bone pain, fatigue, or kidney issues start to appear, and treatment becomes necessary.
- Plasmacytoma: Localized growth of cancerous plasma cells that appear in a single area, either in the bone or soft tissue.
- Light Chain Amyloidosis: A related condition where misfolded proteins build up in organs like the heart or kidneys, disrupting how they work.
Symptoms of Blood Cancer:
Blood cancer symptoms are often subtle or mistaken for other less serious conditions. Common signs include:
- Fever
- Pale skin
- Fatigue and weakness
- Frequent infections
- Swollen lymph nodes
- Easy bruising or bleeding
- Bone pain or tenderness
- Joint pain
- Night sweats
- Shortness of breath
- Unexplained weight loss
- Enlarged liver or spleen
If these symptoms last more than 2-3 weeks, consult your nearest healthcare provider.
Causes of Blood Cancer:
Blood cancer usually starts with a mutation in the DNA of blood-forming cells. DNA acts like a control center, guiding cells on when to grow, divide, or die.
But when these instructions are faulty, cells can grow uncontrollably and live much longer than they are needed. Over time, these abnormal cells take over the bone marrow and crowd out healthy blood cells.
This disruption affects the body’s ability to fight infections, carry oxygen, and form clots: essential for stopping blood loss and wound healing.
Risk Factors You Should Know
Several factors may increase your chances of developing blood cancer:
- Age: Most cases are diagnosed in older adults, especially over 60.
- Gender: Men are statistically more likely to be diagnosed than women.
- Smoking: Tobacco toxins can damage bone marrow and raise the risk of leukemia.
- Chemical Exposure: Prolonged exposure to industrial chemicals like benzene or formaldehyde may contribute.
- Past Cancer Treatments: Chemotherapy or radiation therapy can increase future risk.
- Family History: In rare cases, inherited genetic mutations or a close relative with blood cancer may slightly raise the odds.
- Chronic Immune Conditions: Autoimmune diseases or organ transplants can weaken the immune system and create risk.
- Certain Viral Infections: Viruses like HIV, EBV, or HTLV-1 have been linked to specific types of blood cancers.
Is Blood Cancer Preventable?
There’s no surefire way to prevent blood cancer. Many people with no known risk factors still develop it.
However, avoiding smoking, minimizing chemical exposure, and staying proactive on chronic health issues can reduce risk.
Differences Between Leukemia, Lymphoma, and Myeloma:
Leukemia, lymphoma, and myeloma are all hematologic malignancies (blood cancers) but differ in their site of origin, cell types involved, and clinical manifestations. Understanding the differences between leukemia, lymphoma and myeloma is crucial for accurate diagnosis and treatment planning.
- Leukemia disrupts normal blood cell production
- Lymphoma impacts immune function via lymphatic tumors
- Myeloma damages bones, kidneys, and immune function via abnormal plasma cell
All three need different diagnostic approaches and treatments. Some treatments may overlap (e.g., stem cell transplant), but the approach really depends on the specific type and how early it’s caught. Getting diagnosed early and choosing the right treatment can make a huge difference.
Which Type of Blood Cancer is the Most Dangerous?
Among all types, acute leukemias, especially Acute Myeloid Leukemia (AML), are often considered the most dangerous. They grow fast and can become serious within weeks if not treated.
Multiple Myeloma can also be tough to manage. It’s harder to cure and often comes back after treatment.
On the other hand, chronic blood cancers like Chronic Lymphocytic Leukemia (CLL) or Chronic Myeloid Leukemia (CML) grow slowly and are more manageable, but they can still become aggressive over time.
Which type of blood cancer is the most dangerous? While all forms have serious implications, aggressive cancers like AML and advanced myeloma typically pose the greatest threat, especially when diagnosis is delayed.
Stages of Blood Cancer
Unlike solid tumors, blood cancers don’t always follow a clear staging system, but doctors do use classification systems to describe how advanced the cancer is. Staging often depends on the type of blood cancer you have.
For Leukemia: Leukemia is typically categorized as acute or chronic, and staging is based on blood counts, the percentage of abnormal cells in the bone marrow, and symptoms.
For Lymphoma: A staging system from Stage I to IV is used:
- Stage I: Cancer is in one lymph node region or one nearby organ.
- Stage II: Cancer is in two or more lymph node areas on the same side of the diaphragm.
- Stage III: Cancer is in lymph nodes on both sides of the diaphragm.
- Stage IV: Cancer has spread to organs like the liver, bone marrow, or lungs.
For Multiple Myeloma: Doctors use the Revised International Staging System (R-ISS) which looks at factors like:
- Levels of certain proteins in the blood
- Genetic markers
- How well your kidneys are functioning
Your stage helps guide your treatment plan and gives insight into long-term outlook.
Blood Cancer Survival Rates
| Type of Blood Cancer | Average 5-Year Survival Rate | Notes |
|---|---|---|
| Chronic Lymphocytic Leukemia (CLL) | ~85% | Often slow-growing and manageable with treatment. |
| Acute Lymphoblastic Leukemia (ALL) | ~70% (adults), ~90% (children) | Higher survival in children; treatment depends on age and risk factors. |
| Chronic Myeloid Leukemia (CML) | ~70%–80% | Targeted therapies have significantly improved outlook. |
| Acute Myeloid Leukemia (AML) | ~30% | Aggressive; survival depends heavily on age and treatment response. |
| Hodgkin Lymphoma | ~89% | Highly treatable, especially when caught early. |
| Non-Hodgkin Lymphoma | ~74% | Varies widely based on subtype and stage. |
| Multiple Myeloma | ~57% | Still considered incurable, but newer therapies are extending survival. |
Source: American Cancer Society and other trusted oncology research data (as of 2024).
Is Blood Cancer Hereditary?
In most cases, blood cancer is not hereditary. It usually happens due to changes in your DNA over time. But in rare cases, it can run in families due to inherited genetic mutations.
Living with Blood Cancer:
Dealing with blood cancer can feel overwhelming, but having the right information helps you to make informed decisions. Understanding the types, symptoms, and treatment options gives you the clarity to move forward.
Ongoing advances in oncology research are leading to more effective and personalized treatments. Many patients now benefit from oncology cancer clinical trials, which offer access to innovative therapies that aren’t yet widely available. If you’re considering this option, clinical trial recruitment programs help you match with studies tailored to your condition.
Early diagnosis, the right support, and access to the latest advancements can make a real difference.